ACL Reconstruction
Common Misconceptions about ACL Reconstruction: Debunking Myths
by admin
28th August 2023
6 minutes read
Introduction
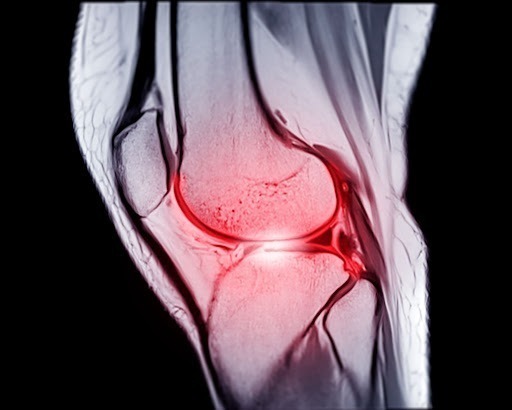
Anterior cruciate ligament (ACL) reconstruction is a surgical procedure that repairs a torn or damaged ACL, one of the key ligaments in the knee. This procedure is often necessary following a sports-related injury or other physical trauma that results in an unstable knee, severe pain, or inability to participate in athletic activities.
The process typically involves the following steps:
- Anesthesia: The patient is put under general anesthesia to prevent pain during the procedure. In some cases, regional anesthesia may be used instead.
- Removal of the damaged ACL: The surgeon makes small incisions around the knee and uses special instruments to remove the damaged ligament.
- Graft Preparation: The new ligament, or graft, is typically taken from the patient’s own body (autograft), usually from the patellar tendon, hamstring tendon, or quadriceps tendon. Alternatively, it may come from a donor (allograft).
- Graft Placement: The surgeon drills holes into the femur (thigh bone) and tibia (shin bone) at the locations where the ACL attaches. The graft is then threaded through these holes to replace the old ACL.
- Securing the Graft: The graft is secured with screws or other fixation devices. The exact method used can depend on the specific circumstances of the surgery and the type of graft used.
- Closure and Recovery: The incisions are then closed, and the knee is usually immobilized initially with a brace. The patient begins a rehabilitation program to restore strength and stability to the knee.
Success rates for ACL reconstruction are generally quite high, with many people returning to their previous levels of activity after surgery. However, like all surgical procedures, there are risks, including infection, blood clots, graft failure, and the continued instability or stiffness in the knee.
Myths and Facts on ACL Reconstruction Surgery
Myth 1: ACL Reconstruction is Necessary for All ACL Injuries
Fact: Not all ACL injuries require surgery. Some partial tears or minor ACL injuries may heal with conservative treatments, such as physical therapy and bracing. The decision for ACL reconstruction depends on the individual’s lifestyle, activity level, and the degree of knee instability.
Myth 2: ACL Surgery is a Quick Fix
Fact: ACL reconstruction is not a quick fix, and the recovery process can be lengthy. It requires a comprehensive rehabilitation program to regain strength, stability, and knee function fully. Patients must be patient and committed to following their physical therapist’s instructions to achieve successful outcomes.
Myth 3: ACL Surgery is Always Painful
Fact: While post-operative pain is expected after ACL surgery, advancements in surgical techniques and pain management have significantly reduced pain levels. Pain can be managed effectively with prescribed medications, ice therapy, and rest during the initial recovery period.
Myth 4: Athletes Must Get ACL Reconstruction to Return to Sports
Fact: While ACL reconstruction is often recommended for athletes who wish to return to high-intensity sports, some athletes with partial tears or low-demand activities may not require surgery. The decision for ACL reconstruction should be individualized based on the patient’s goals and lifestyle.
Myth 5: Only Professional Athletes Need ACL Reconstruction
Fact: ACL injuries can occur in athletes of all skill levels, as well as in non-athletes involved in everyday activities. ACL reconstruction is recommended for anyone who experiences knee instability and wishes to maintain an active lifestyle, regardless of their athletic level.
Myth 6: ACL Surgery Leads to Arthritis
Fact: While it is true that some ACL injury cases can lead to early-onset osteoarthritis, ACL reconstruction has been shown to reduce the risk of arthritis in the long term. Proper rehabilitation and adherence to post-operative guidelines can help protect the knee joint and reduce the risk of arthritis.
Myth 7: Arthroscopic ACL Reconstruction is Riskier than Open Surgery
Fact: Arthroscopic ACL reconstruction is a minimally invasive procedure with smaller incisions, leading to reduced tissue damage, less pain, and faster recovery compared to open surgery. The risk of complications is generally lower with arthroscopic techniques.
Myth 8: ACL Reconstruction is Not Suitable for Older Adults
Fact: Age alone is not a determining factor for ACL reconstruction candidacy. Older adults who are physically active and experience knee instability may benefit from ACL reconstruction. The surgeon will consider individual health factors and lifestyle when making the recommendation.
Myth 9: ACL Grafts From Donors are Inferior to Autografts
Fact: Both autografts (using the patient’s tissues) and allografts (using donor tissues) have shown successful outcomes in ACL reconstruction. The choice of graft depends on the surgeon’s preference, patient factors, and the patient’s activity level.
Myth 10: ACL Surgery Makes the Knee “Good as New”
Fact: While ACL surgery can significantly improve knee stability and function, it does not make the knee entirely “good as new.” Some individuals may experience mild residual symptoms, and it is essential to continue injury prevention strategies and exercise regularly to maintain knee health.
Conclusion
ACL reconstruction surgery is a well-established and successful procedure for treating ACL injuries and restoring knee stability. It is essential to dispel common misconceptions and myths surrounding ACL reconstruction to provide accurate information to patients considering the procedure. While ACL surgery is not necessary for all ACL injuries and recovery requires dedication, it can significantly improve knee function and quality of life for athletes and active individuals. Patients should work closely with their orthopedic surgeon and physical therapist to understand the best treatment approach for their specific condition and achieve successful outcomes after ACL reconstruction.
How Can Medfin Help?
Medfin is a daycare surgery expert providing access to the latest surgical procedures and top doctors in your city at affordable prices. Medfin provides you access to top doctors in bangalore with 10+ years of experience. With Medfin, you can leave your hassles behind and focus on your health. From instant consultations to paperwork assistance, we have got you covered with everything. So why wait? Call us today!
FAQs
1. What are the symptoms of an ACL injury?
Symptoms of an ACL injury include a popping sound at the time of injury, immediate and severe pain, swelling within a few hours, instability in the knee (feeling of the knee “giving way”), and limited range of motion.
2. Can ACL injuries heal on their own?
ACL tears do not typically heal on their own due to the ligament’s limited blood supply. Conservative treatments like rest, physical therapy, and bracing may be sufficient for individuals with a partially torn ACL who do not require significant knee stability.
3. Is surgery necessary for ACL injury treatment?
For athletes and active individuals or those with significant instability and functional limitations, ACL reconstruction surgery is often recommended. It involves replacing the torn ACL with a graft from the patient’s own tissues (autograft) or a donor (allograft).
4. How long does it take to recover from ACL reconstruction surgery?
Recovery time varies, but most patients can begin walking with support a few days after surgery. Full recovery and return to sports may take six months to a year, depending on individual progress and adherence to rehabilitation guidelines.
5. What is the success rate of ACL reconstruction surgery?
ACL reconstruction has a high success rate, with many patients achieving excellent long-term outcomes and restoring knee function. However, success depends on factors like patient compliance with rehabilitation and the skill of the surgeon.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
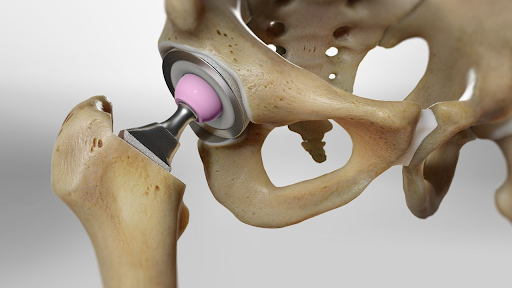
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
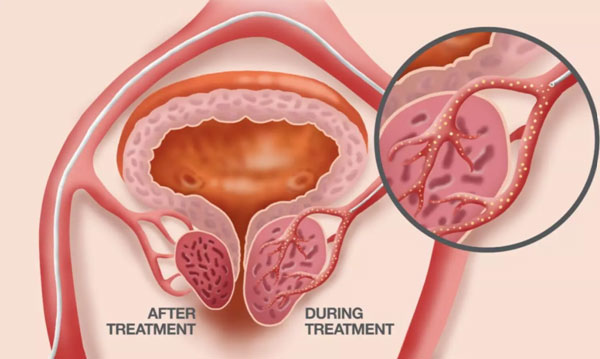
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS