Urology
Why is Ureteroscopy Done by Urologists and Nephrologists?
by admin
29th September 2023
8 minutes read
Introduction
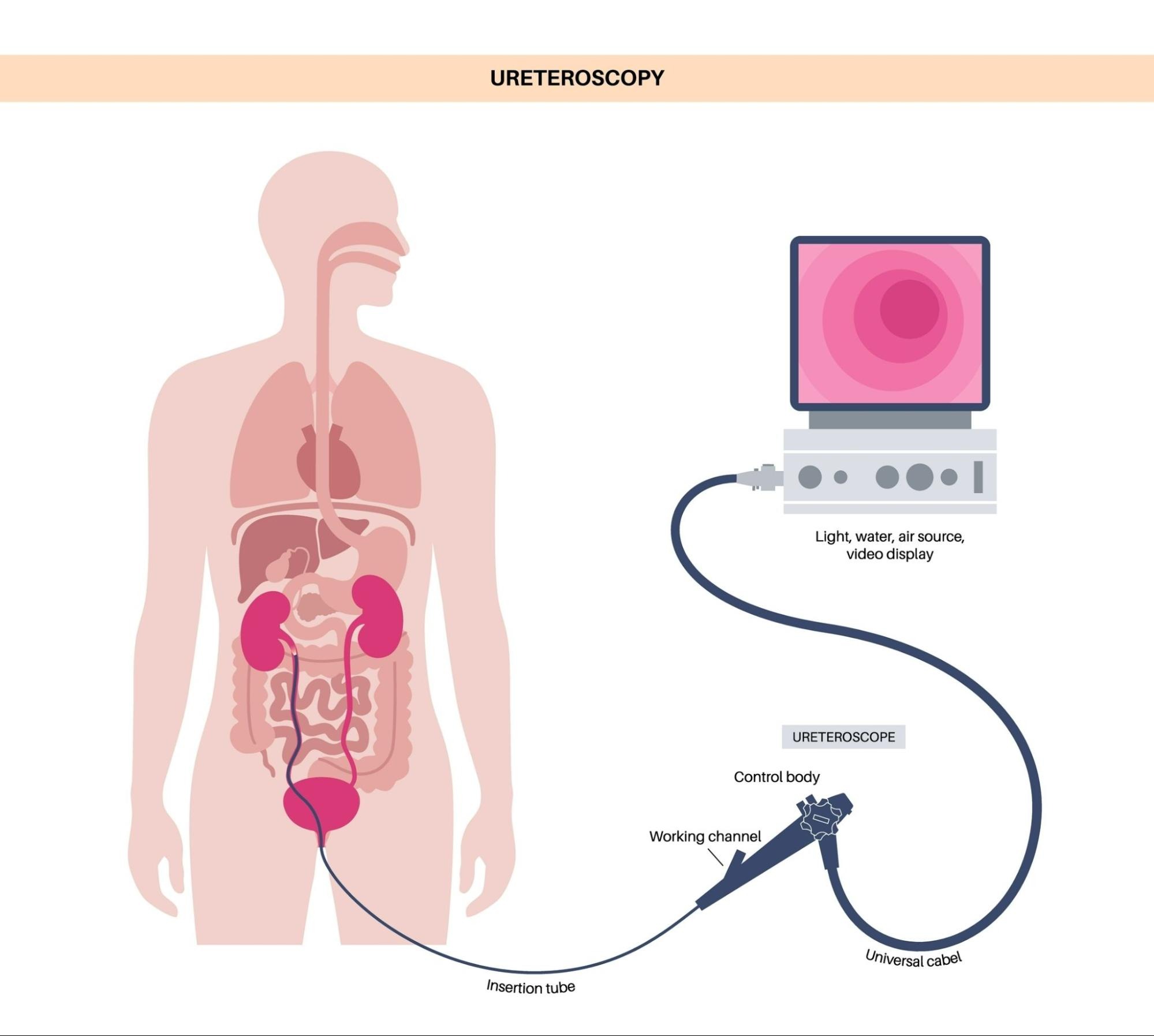
Ureteroscopy is a diagnostic and therapeutic procedure conducted by urologists and nephrologists to examine, treat, or relieve obstructions in the ureters (the tubes connecting the kidneys to the bladder). The process involves inserting a thin, flexible scope into the urethra, through the bladder, and into the ureters to visualize and address issues such as kidney stones, strictures, or tumors. This minimally invasive technique provides a direct view, enabling the precise management of ureteral and renal disorders. Through ureteroscopy, healthcare practitioners not only diagnose conditions accurately but also perform necessary interventions, like stone removal or biopsy, which are crucial for maintaining the urinary tract’s functionality and the patient’s overall renal health.
Urologists vs. Nephrologists: Roles and Specializations
Urologists and nephrologists are both medical specialists who focus on different aspects of the urinary system. While there may be some overlap in their areas of expertise, they have distinct roles and specializations.
1. Role of Urologists:
- Urologists primarily deal with the surgical and medical management of disorders related to the urinary tract system in both males and females.
- They diagnose and treat conditions such as urinary tract infections, kidney stones, bladder problems, prostate issues (such as enlarged prostate or prostate cancer), erectile dysfunction, infertility, and other urological cancers.
- Urologists also perform surgeries involving the urinary tract system, including procedures like ureteroscopy, cystoscopy, prostatectomy, kidney transplantation, and various forms of reconstructive surgery.
2. Role of Nephrologists:
- Nephrologists specialize in the diagnosis and treatment of diseases that affect the kidneys specifically.
- They manage conditions like chronic kidney disease (CKD), acute kidney injury (AKI), glomerulonephritis, polycystic kidney disease (PKD), kidney infections, electrolyte imbalances, hypertension-related kidney problems, and renal failure.
- Nephrologists are responsible for evaluating kidney function through various tests like blood work, urine analysis, imaging studies (such as ultrasounds or CT scans), and performing kidney biopsies when necessary.
- They provide non-surgical treatments such as medication management, dialysis (hemodialysis or peritoneal dialysis), pre-and post-transplant care for patients undergoing kidney transplantation.
In summary, urologists focus on both surgical and medical management of disorders throughout the entire urinary tract system (including reproductive organs in males), while nephrologists specialize in diagnosing and treating diseases that specifically impact the kidneys.
Kidney Stones and Ureteroscopy
Kidney stones are hard mineral deposits that form in the kidneys and can cause severe pain and discomfort. Ureteroscopy is a minimally invasive procedure used to remove kidney stones from the ureters or the kidneys. During the procedure, a thin tube with a camera attached (ureteroscope) is inserted through the urethra and guided into the urinary tract. Once located, the stone can be broken up using laser energy or removed entirely using small instruments. Ureteroscopy has become a popular treatment option due to its high success rate and minimal recovery time compared to traditional open surgery.
Role Of Urologists in Ureteroscopy
Urologists play a crucial role in performing ureteroscopy, a minimally invasive procedure used to diagnose and treat conditions affecting the urinary tract. Here are some key roles urologists have in ureteroscopy:
1. Diagnosis:
Urologists use ureteroscopy to visually inspect the ureters and kidneys for any abnormalities such as stones, tumors, strictures, or other conditions that may cause urinary tract symptoms.
2. Stone removal:
Urologists commonly perform ureteroscopy to remove kidney stones or fragments that have not passed naturally through the urinary system. They use specialized tools to break down larger stones into smaller pieces and then extract them using tiny baskets or graspers.
3. Biopsy:
If there is suspicion of cancer or abnormal tissue growth within the urinary tract during ureteroscopy, urologists can take small tissue samples (biopsies) for further examination under a microscope. This helps in diagnosing and staging various urological cancers.
4. Treatment of strictures:
Ureteral strictures (narrowing of the ureters) can occur due to various reasons such as previous surgeries, infections, or inflammation. Urologists can use ureteroscopy to visualize these strictures and perform procedures like balloon dilation or placement of stents to widen the narrowed segments.
5. Stent placement and removal:
In cases where temporary relief is needed for blockages or after stone removal, urologists may place a thin tube called a stent inside the urinary tract via ureteroscopy. These stents help keep the urine flowing properly until further treatment can be provided. Urologists are also responsible for removing these stents once they are no longer required.
6. Treatment of tumors:
Ureteroscopy allows urologists to visualize tumors within the urinary tract and guide surgical instruments for their removal or biopsy. This technique is particularly useful for early-stage tumors and can help avoid more invasive procedures.
7. Post-operative care:
Urologists are responsible for providing comprehensive post-operative care following ureteroscopy. They monitor patients for any complications, manage pain, prescribe medications, and provide guidance on recovery and follow-up plans.
In summary, urologists play a vital role in the diagnosis, treatment, and management of various urinary tract conditions through ureteroscopy. Their expertise in performing this procedure helps ensure optimal outcomes for patients with urinary tract disorders.
Involvement of Nephrologists in Ureteroscopy
Nephrologists may be involved in ureteroscopy in several ways:
1. Preoperative evaluation:
Nephrologists may be consulted to evaluate the kidney function and electrolyte balance of patients before undergoing ureteroscopy. This is particularly important for patients with pre-existing kidney diseases or risk factors for renal impairment.
2. Management of medical conditions:
Nephrologists may manage underlying medical conditions that can affect the outcome of ureteroscopy, such as hypertension, diabetes, or chronic kidney disease. They may adjust medications or provide guidance on optimizing the patient’s overall health status prior to the procedure.
3.Perioperative care:
Nephrologists may collaborate with urologists during the perioperative period to ensure adequate hydration, monitor electrolyte levels, and manage fluid and diuretic therapy. They may also provide input on the choice of anesthesia, especially for patients with renal impairment.
4. Complication management:
In case complications arise during or after ureteroscopy that affect kidney function, nephrologists play a crucial role in managing these complications. They may provide recommendations for appropriate interventions or adjustments in treatment plans to mitigate further kidney damage.
5. Follow-up care:
Nephrologists may participate in post-operative care by monitoring kidney function, assessing any changes in electrolyte balance, and providing long-term management of any renal issues that arise from the procedure.
Overall, nephrologists have an important role in ensuring optimal outcomes for patients undergoing ureteroscopy by managing their pre-existing medical conditions and closely monitoring their kidney function throughout the process.
When do urologists and nephrologists work together on kidney stone management?
Urologists and nephrologists often work together on kidney stone management in several scenarios, including:
1. Complex cases:
When a patient has complicated or recurrent kidney stones, both specialists collaborate to develop an appropriate treatment plan. This may involve determining the underlying causes of stone formation and implementing preventive measures.
2. Surgical intervention:
Urologists are typically responsible for performing surgical procedures to remove kidney stones, such as ureteroscopy, shock wave lithotripsy (SWL), or percutaneous nephrolithotomy (PCNL). Nephrologists may provide pre- and post-operative care, manage any associated medical conditions, and offer guidance regarding fluid intake, dietary modifications, and medication management.
3. Metabolic evaluation:
Nephrologists specialize in evaluating metabolic factors that contribute to kidney stone formation. They perform comprehensive metabolic evaluations to identify any underlying disorders like hypercalciuria, hyperoxaluria, or cystinuria. Based on these findings, they can recommend lifestyle changes or prescribe medications to prevent further stone development. Urologists then coordinate with nephrologists to implement these preventive measures.
4. Chronic kidney disease (CKD):
Kidney stones can sometimes lead to CKD if left untreated or managed poorly. In such cases, nephrologists play a crucial role in monitoring the patient’s renal function and managing any complications arising from the presence of stones. Urologists work alongside nephrologists to address the specific urological aspects of kidney stone management while ensuring overall renal health.
5. Referral system:
Primary care physicians often refer patients with kidney stones to both urologists and nephrologists simultaneously for specialized care and a comprehensive approach to treatment.
The collaboration between urologists and nephrologists ensures that patients receive a holistic approach to kidney stone management by addressing both urological concerns related to stone removal and medical considerations for prevention and long-term kidney health.
Conclusion
Ureteroscopy stands as a cornerstone procedure in diagnosing and treating kidney stones, providing a minimally invasive, effective avenue for urologists to manage urinary tract obstructions. Through this technique, practitioners can offer prompt relief from painful symptoms and potentially prevent recurrence by analyzing stone composition. The advancements in endoscopic technology have further propelled ureteroscopy to be a standard, often outpatient, procedure with quicker recovery timelines, solidifying its pivotal role in contemporary urological care.
FAQs
Ureteroscopy is usually performed under general or spinal anesthesia to ensure the patient remains still and comfortable throughout the procedure.
The procedure typically takes 1 to 2 hours, but the duration may vary based on the complexity of the condition.
Yes, besides treating kidney stones, ureteroscopy can be used to treat ureteral strictures, and tumors, or to retrieve dropped ureteral stents.
The success rate is high, often above 90%, but varies based on factors like stone size, location, and surgeon experience.
Some discomfort or mild pain is common post-procedure, often managed with over-the-counter pain relievers or prescribed medications.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
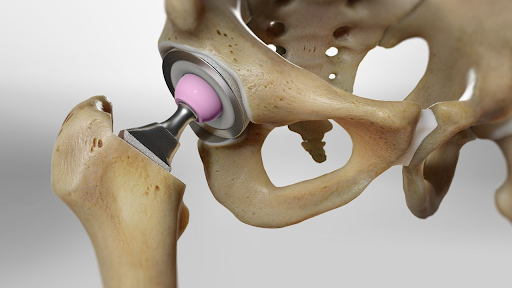
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
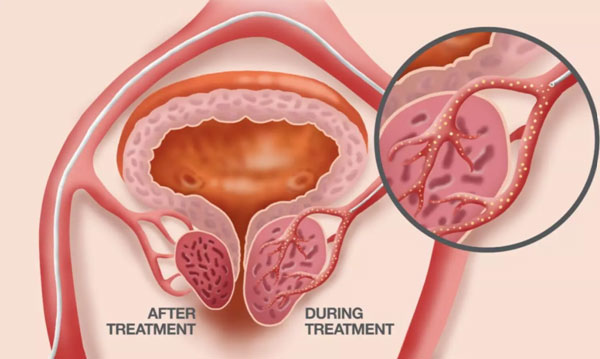
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS