Urology
Why Is The Penis Glans Over-Sensitive Or Painful If You Have Phimosis?

by admin
30th October 2023
8 minutes read
Phimosis is a condition when the foreskin cannot entirely retract over the head of the penis. Oversensitivity or even discomfort in the penis glans is a typical sign. But why does this occur? This blog explores the underlying causes of this increased sensitivity and pain, illuminating the complex interplay between phimosis and glans sensitivity.
What is Phymosis?
Phimosis is a physical condition where the person, typically a male, cannot retract the foreskin over the external gland. It is relatively common in younger boys and usually resolves on its own. In the case of older males, the condition may be present abated over many years, causing pain, discomfort, or hygiene problems. The condition occurs due to numerous reasons. Recurrent inflammation, infection, trauma, or scarring are the reasons behind phimosis.
What are the Causes and Risk Factors of Phymosis?
Phimosis can have many different root causes and may be affected by a number of risk factors, including
Causes of Phimosis:
- Congenital phimosis: A natural condition in which the boy is born with a foreskin that is tight and can’t be pulled back. As they get older, it usually loosens, so that by puberty, retraction is normal.
- Scarring: Trauma or repeated infections can lead to scarring of the foreskin. This can make it hard or impossible to pull the foreskin back.
- Balanitis: This is an inflammation of the glans (the tip of the penis). When it keeps happening, it can lead to scarring of the foreskin which then causes phimosis.
- Posthitis: This inflammation of the foreskin can lead to phimosis either by the swelling associated with it or because repeated episodes cause scarring.
- Poor hygiene: Failing to clean under the foreskin properly on a regular basis can cause infections. These can lead to scarring and make the foreskin become tight
Risk Factors:
- Age: The foreskin of young boys is often naturally non-retractable. This is typically considered normal and often resolves by the time a boy reaches adolescence.
- Infections: Conditions such as balanoposthitis put someone at higher risk.
- Medical conditions: Diabetes can increase the risk of infections in the genital area, potentially contributing to the development of phimosis. Likewise, certain other conditions, such as having a weakened immune system, make someone more susceptible to infections that can lead to phimosis.
- Use of catheters: Frequent insertion of urinary catheters for other conditions can risk injury or infection in the opening of the penis, potentially leading to the development of phimosis.
- Forceful retraction: Trying to forcefully retract the foreskin before it’s ready, usually after age 3, can cause scarring and lead to phimosis later.
- Poor hygiene: Not cleaning beneath the foreskin on a regular basis can cause a collection of smegma, which can lead to infection and, subsequently, phimosis.
The Glans and Sensitivity
The glans or head of the penis is a highly sensitive area due to the presence of many nerve endings. When the foreskin is unable to retract properly, as in the case of phimosis, it can cause the glans to be exposed to constant friction and stimulation, which may lead to heightened sensitivity.
Symptoms of Glans Sensitivity in Phimosis
- Hypersensitivity: The glans is often highly sensitive to any touch or pressure, especially if it has been exposed after being covered for a long period of time.
- Pain or Discomfort: Any direct contact with the glans usually will cause some pain such as during bathing, sexual activity, or if rubbed by friction against clothing because of the increased sensitivity of the glans.
- Difficulty with Sexual Activity: The poor hygiene habits and the hyped level of sensitivity make the sexual activities, like masturbation or intercourse, uncomfortable or painful; pain can also be felt when you are trying to stretch the foreskin or the friction at the time of intercourse may also intensify the situation.
- Burning or Stinging Sensation: The glans sometimes may experience a burning or stinging sensation, especially if it is exposed to irritants like soap or other chemicals; irritation can also increase because of these kinds of chemicals.
- Difficulty or Pain While Urinating: The urinating typically might also become very uncomfortable for you if the stream of urine directly contacts the hypersensitive glans there by urine touching the edge of the foreskin and then leaking to the glans.
- Redness or Swelling: If the glans has been exposed to irritants or excessive rubbing, it may seem red or somewhat swollen.
- Ballooning of the Foreskin: When you urinate, the phimotic foreskin may balloon out with the backflow of trapped urine which creates increased pressure on the sensitive, glans.
- Bleeding or Cracking: If the tight foreskin is forcibly retracted, the ridged band may get cracks or tears due to the grinding between the glans and the ridged band which may cause minor bleeding and increased glans sensitivity.
How is Phymosis Treated?
The treatment options for phimosis depend on factors such as the cause of phimosis, the age of the individual, and the severity of the condition. The treatment options include the following:
- Watchful waiting: Many boys have physiological phimosis, and the condition will resolve as they grow. No specific treatment is necessary unless there are problems such as recurrent infection or difficulty with urination.
- Topical steroids: Applying a corticosteroid cream or ointment to the foreskin may reduce inflammation and help the skin retract more easily. A provider can prescribe such a cream, and parents will apply it to the foreskin.
- Stretching exercises: Gentle retraction of the foreskin can gradually increase elasticity, but the procedure must be done carefully to avoid injury and discomfort. Steroid creams and careful retraction are often used together in treatment.
- Preputioplasty: A simple surgical procedure, preputioplasty involves a longitudinal incision of the foreskin with transverse sutures to expand the opening . No tissue is removed; only the opening in the foreskin is expanded to make retraction easier.
- Circumcision: The surgical removal of the foreskin is the definitive treatment for phimosis, but it is usually reserved for situations in which other treatments have failed or are not appropriate, such as recurrent infection or severe scarring.
- Treatment of Underlying Issues: The medical treatment of underlying causes such as infections or other conditions is a primary approach, or can be adjunctive to these approaches. Such treatment may include antibiotics for bacteria or treatment of conditions such as balanitis.
Phimosis: Preventive Measures
While some cases of phimosis are physiologic and resolve spontaneously as the child grows older, others are the result of factors that may be preventable. There are some measures that may help to prevent phimosis or its complications:
- Gentle Cleaning: Educate on gently cleaning below the foreskin to prevent smegma from accumulating but discourage forcible retraction of the foreskin, especially in young boys, which can cause injury to the foreskin and scarring.
- Avoidance of Irritants: Cautions should be given to not using harsh soaps, lotions, and other products on the penis that could cause inflammation of the penis and the foreskin.
- Educate on Proper Foreskin Care: Parents should be taught that the foreskin of infants and young boys should be left alone and never forcibly retracted. The foreskin separates from the glans naturally with time.
- Prompt Treatment of Infections: Advise patients to come in right away for any sign of infection, including redness, swelling, pain or discharge, to prevent any infection, such as Balanitis, from causing enough swelling to result in phimosis.
- Protect Against Trauma: Caution patients to protect against trauma to the penis to avoid trauma-related phimosis.
- Safe Sexual Practices: Safe sex helps to avoid sexually transmitted infections (STIs), such as balanitis and posthitis, which increase the likelihood of phimosis.
- Moisturizers and Lubricants: For dryness or mild irritation, a mild moisturizer may be helpful. Lubricants can also be helpful during sexual activity to reduce friction and the chance of trauma.
FAQs
Directly, phimosis does not affect a man’s ability to produce sperm and thus his fertility. However, if it causes pain or difficulty during intercourse, it might indirectly impact sexual activity and conception.
While chronic inflammation or infections associated with phimosis might increase the risk of penile cancer, phimosis itself is not a direct cause. Regular check-ups and good hygiene can help mitigate the risk.
It’s essential to consult a healthcare professional before applying any medication. Over-the-counter creams might not be effective and could worsen the condition or cause side effects.
While phimosis itself is not a direct cause of ED, the pain and discomfort associated with the condition might affect sexual function. Additionally, psychological distress from phimosis might contribute to ED in some individuals.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
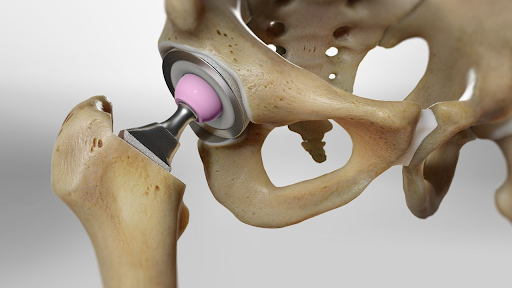
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS