Urology
Understanding Two Common Penis Disorders: Phimosis and Paraphimosis

by admin
4th October 2023
9 minutes read
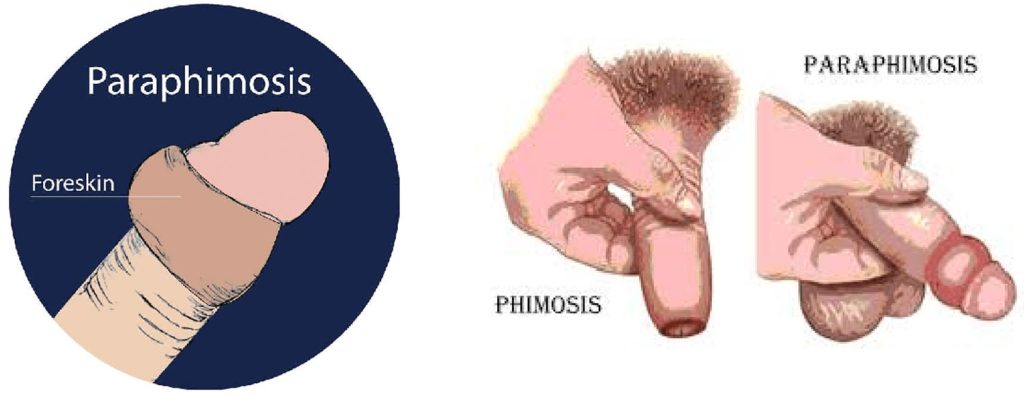
What is Phimosis?
Phimosis is a condition where the foreskin of the penis cannot be fully retracted over the glans (head) of the penis. It can be physiological (normal) or pathological.
1.Physiological Phimosis:
This is the normal condition in which many baby boys are born. Their foreskin is naturally tight and adherent to the glans. Over time, this adhesion gradually breaks down, allowing the foreskin to retract. By puberty, most males are able to fully retract their foreskin. Thus, physiological phimosis is generally not a cause for concern and often resolves on its own.
2. Pathological Phimosis:
This occurs when the foreskin cannot be retracted due to scarring, inflammation, or other medical reasons. This can lead to discomfort, pain, and other complications.
Causes of Pathological Phimosis:
- Scarring: Repeated episodes of foreskin infections or trauma can lead to scarring, which can cause the foreskin to become non-retractable.
- Balanitis: This refers to inflammation of the glans, which can sometimes extend to the foreskin, leading to phimosis. It can be caused by infections, irritants, or other conditions.
- Balanoposthitis: Inflammation of both the glans and the foreskin.
- Lichen Sclerosus (BXO – Balanitis Xerotica Obliterans): This is a skin condition that can affect the genital area, causing a white, patchy appearance and can lead to phimosis due to scarring.
- Recurrent Infections: Chronic or repeated yeast infections or other types of infections can cause inflammation and scarring, leading to phimosis.
- Poor Hygiene: Not cleaning under the foreskin can result in infections and subsequent scarring.
- Age: In older men, the foreskin can become less elastic and harder to retract.
What are the Symptoms of Phimosis?
Phimosis can be asymptomatic, especially when it’s physiological in nature (e.g., in young boys where it’s considered normal). However, when symptoms do occur, they can include:
- Difficulty retracting the foreskin: This is the primary symptom. In mild cases, the foreskin can be retracted with some effort, but in severe cases, it may be impossible to expose the glans (head) of the penis.
- Tight foreskin with a constricted appearance: The end of the foreskin may look like a narrow ring, which can become more evident when the penis is erect.
- Pain or discomfort: This can be experienced during erection, sexual activity, or urination.
- Swelling or redness: Especially at the tip of the penis.
- Ballooning of the foreskin during urination: This occurs when urine gets trapped under the unretractable foreskin, causing it to balloon outwards.
- Discharge or odor: Due to infections or poor hygiene underneath the foreskin.
- Painful erections: The tight foreskin can constrict the penis during an erection.
- Bleeding: Especially if there are micro-tears in the foreskin.
Diagnosis and Treatment of Phimosis
The diagnosis of phimosis is primarily clinical, based on a physical examination and patient history. The doctor will:
- Inspect the penis: To assess the degree to which the foreskin can be retracted and to look for any signs of inflammation, scarring, or other abnormalities.
- Ask about symptoms: Such as pain during urination, painful erections, or any other related symptoms.
- Determine the type of phimosis: Whether it’s physiological (common in young boys) or pathological (due to scarring or another cause).
In some cases, if there’s a concern about an underlying skin condition (e.g., lichen sclerosus) or if infections are recurrent, the doctor might take a swab or biopsy for further investigation.
Treatment of Phimosis:
The treatment approach varies based on the severity of the phimosis, the patient’s age, and the presence of symptoms.
1. Observation: If the phimosis is physiological and does not cause any problems, no treatment may be necessary. The doctor might recommend periodic follow-ups to monitor the condition.
2. Topical Steroids: Applying a topical steroid cream to the foreskin can help in some cases, especially if there is no scarring. This treatment can soften the skin and increase its elasticity, allowing for easier retraction. It is usually applied once or twice daily for a few weeks.
3. Gentle Retraction: Over time, gentle and gradual retraction can help stretch the foreskin. This should never be forceful, as it can lead to tears and subsequent scarring.
4. Good Hygiene: Regular cleaning beneath the foreskin can prevent infections and associated complications.
5. Surgery:
- Circumcision: This is the surgical removal of the foreskin. It’s a definitive solution for phimosis but is more invasive than other options.
- Preputioplasty: This is a less radical surgical procedure than circumcision. It involves making a longitudinal incision in the tight foreskin and then suturing it transversely, which allows the foreskin to retract more easily.
- Frenuloplasty: If the tightness is due to a short frenulum (the band of tissue connecting the underside of the penis head to the foreskin), this procedure lengthens it.
What is Paraphimosis?
Paraphimosis is a urological emergency in which the foreskin, once retracted behind the glans penis, cannot be returned to its original position to cover the glans. If left untreated, paraphimosis can restrict blood flow to the glans and lead to tissue death or gangrene.
Causes of Paraphimosis:
- Forceful Retraction: Paraphimosis can occur if the foreskin is forcefully retracted and not returned to its original position, either inadvertently or intentionally.
- Medical Procedures: If the foreskin is pulled back during a procedure (e.g., catheter insertion) and not returned to its original position afterward.
- Sexual Activity: If the foreskin is retracted during sexual activity and not returned afterward.
- Piercings: Genital piercings involving the foreskin can sometimes lead to paraphimosis if they cause the foreskin to remain retracted.
- Swelling: Any condition or infection that causes the foreskin or the glans to swell can make it difficult to move the foreskin back to its normal position.
- Underlying Scarring or Tight Foreskin: A previously tight or scarred foreskin may increase the risk of paraphimosis if it’s retracted.
What are the Symptoms of Paraphimosis?
Paraphimosis is characterized by specific symptoms, and recognizing them early is crucial due to the potential risk of compromised blood flow to the glans penis. The symptoms include:
- Swollen Glans: The head (glans) of the penis appears swollen, enlarged, and may be painful.
- Constricting Band: A tight band of the foreskin can be seen behind the glans, constricting it and preventing the foreskin from returning to its original position.
- Pain and Discomfort: The affected area can be painful, especially when touched or manipulated.
- Discoloration: As blood flow becomes restricted, the glans may change color, ranging from red to dark blue or purple, indicating severe blood flow compromise.
- Difficulty Urinating: In some cases, the swelling and pain may make it difficult to urinate.
Diagnosis and Treatment of Paraphimosis
Diagnosis of Paraphimosis:
- Physical Examination: The doctor will inspect the penis to determine the extent of swelling, the presence of the constricting band of foreskin, and the condition of the glans.
- Patient History: The doctor will gather information about how and when the condition started, any preceding activities (like catheterization or sexual activity), and if there were prior episodes.
Treatment of Paraphimosis:
Immediate intervention is required to prevent complications. Treatment methods include:
- Manual Reduction: This is the first line of treatment. The doctor may apply a lubricating jelly and use both hands to compress the swollen glans while pushing the foreskin forward over the glans. This might be done under local anesthesia to reduce pain.
- Osmotic Method: Wrapping the swollen glans with a hypertonic solution-soaked gauze can help draw out the edema fluid, making manual reduction easier.
- Puncture Technique: If manual reduction is not successful, the constricting band can be punctured with a needle in multiple places to relieve the constriction, allowing the foreskin to be moved forward.
- Surgical Intervention: In rare cases where other methods fail or if there is significant tissue damage, surgical intervention might be required. This could involve a dorsal slit (a cut along the top of the foreskin) to relieve the constriction or, in extreme cases, circumcision.
Your doctor may also prescribe antibiotics and pain medications if there’s an associated infection and other related symptoms.
Preventive Methods for Phimosis & Paraphimosis?
Preventing phimosis and paraphimosis primarily revolves around proper penile care, education, and early intervention if issues arise. Here are some preventive methods:
For Phimosis:
- Avoid Forceful Retraction: Never forcibly retract the foreskin, especially in young boys. This can cause micro-tears and subsequent scarring, which can lead to phimosis.
- Good Hygiene: Regular gentle cleaning under the foreskin can prevent infections, which if recurrent, can cause scarring and phimosis. Teach young boys how to clean under their foreskin properly as they reach an age when they can retract it.
- Topical Steroids: In cases where the foreskin starts to become tight but isn’t yet fully phimotic, the application of topical steroids might help increase its elasticity. However, this should only be done under the guidance of a healthcare professional.
For Paraphimosis:
- Educate on Proper Foreskin Care: After retracting the foreskin—for cleaning, examination, or any other reason always ensure that it’s returned to its original position covering the glans.
- Medical Procedures: Healthcare professionals should be diligent about returning the foreskin to its original position after retracting it for medical procedures like catheterization.
- Sexual Education: Men should be educated about the importance of returning the foreskin to its natural position after sexual activity if it has been retracted.
- Prompt Treatment of Swelling: If any swelling or inflammation occurs (from infections or other causes), seek medical advice promptly. This can help prevent a situation where the foreskin is retracted and cannot be returned due to swelling.
Conclusion
Proper penile care and education are crucial in preventing phimosis and paraphimosis. Avoiding forceful retraction, ensuring good hygiene, and returning the foreskin to its natural position after retraction is key. For recurrent issues, consulting a healthcare professional for guidance or potential interventions, including circumcision, can be beneficial.
FAQs
Immediately. Paraphimosis is a urological emergency. Delaying treatment can lead to serious complications.
Yes, if untreated, paraphimosis can restrict blood flow, leading to pain, swelling, and potential tissue death or gangrene of the glans.
Phimosis might cause discomfort or pain during erections or urination. Paraphimosis can be very painful due to the constriction and reduced blood flow.
It can. Phimosis might cause discomfort or pain during sexual activity, potentially affecting performance or pleasure.
Physiological phimosis in young children often resolves on its own as they grow. Pathological phimosis, due to scarring or other causes, usually requires medical intervention.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS