Proctology
Exploring Fistula Treatment Options: A Comprehensive Guide
by admin
25th October 2023
8 minutes read
Introduction
Fistula, an abnormal connection between two body parts, presents a challenging medical condition that necessitates thorough understanding and intervention. The array of treatment options available ranges from simple medications to complex surgeries, largely depending on the fistula’s type, size, and location. This comprehensive guide aims to navigate through the multifaceted landscape of fistula treatment, offering insights into conventional and contemporary approaches.
By exploring medical advancements, analyzing effectiveness, and assessing the post-treatment quality of life, it seeks to provide a well-rounded perspective. This guide will serve as an invaluable resource for those impacted by fistula, ensuring well-informed decision-making in choosing the right treatment pathway.
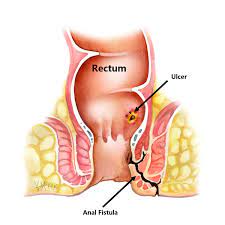
Understanding Fistulas
Fistulas are abnormal passages or connections between two organs or vessels that ordinarily do not connect. They can develop due to injury, surgery, infection, or certain diseases, including Crohn’s disease or diverticulitis. The symptoms anal fistula and severity of a fistula vary based on its location and size, potentially leading to complications like infection or abscess formation. Diagnosis usually involves imaging tests or endoscopic procedures to visualize the fistula. Here let’s understand the management of fistulas in detail.
Management of Fistulas
1. Medications
Medications can be a valuable part of managing fistulas, particularly when they are associated with underlying conditions like inflammatory bowel disease (IBD) or when infection is present. Here are some medications commonly used to help manage fistulas:
- Antibiotics: Antibiotics are prescribed to treat or prevent infection in fistulas, particularly anal or perianal fistulas. They help control bacterial overgrowth and reduce inflammation.
- Biologic Therapies: Biologic medications, such as anti-TNF agents (e.g., infliximab, adalimumab), are used to manage fistulas associated with IBD, like Crohn’s disease. These drugs target specific proteins involved in the inflammatory process, reducing inflammation and promoting healing.
- Immunosuppressive Medications: Corticosteroids, azathioprine, methotrexate, and other immunosuppressive drugs may be used in conjunction with biologics or as standalone treatments for IBD-related fistulas. They help suppress the immune system’s response, reducing inflammation.
- Pain Medications: Pain relievers, such as non-steroidal anti-inflammatory drugs (NSAIDs) or opioids, may be prescribed to manage pain and discomfort associated with fistulas.
- Biologics for Other Conditions: In cases where fistulas are associated with diseases like hidradenitis suppurativa, medications such as adalimumab may be used to manage inflammation and prevent new fistula formation.
The choice of medication depends on the underlying condition, the severity of the fistula, and the patient’s overall health.
2. Minimally Invasive Techniques
Minimally invasive methods for fistula management have revolutionized the treatment of fistulas, offering patients less pain, faster recovery, and improved cosmetic outcomes compared to traditional open surgeries. Some common minimally invasive techniques include:
- Seton Placement: A seton, which is a piece of surgical thread or material, may be placed through the fistula tract. This helps maintain drainage and gradually cuts through the tract to allow for eventual healing.
- Video-Assisted Anal Fistula Treatment (VAAFT): VAAFT is an endoscopic procedure used to treat anal fistulas. A camera-equipped endoscope is inserted into the tract to identify and close the internal opening.
- Ligation of the Intersphincteric Fistula Tract (LIFT): Suitable for high intersphincteric fistulas, LIFT ligates the tract to close the channel.
- Fibrin Glue Injection: Fibrin glue can be injected into certain fistula types to close them.
- Endorectal Advancement Flap Surgery: Healthy rectal tissue is used to cover and close the internal opening.
- Transanal Minimally Invasive Surgery (TAMIS): TAMIS accesses the fistula from inside the rectum using specialized instruments and an endoscope.
Minimally invasive methods offer tailored solutions for various fistula types and locations, improving patient outcomes and quality of life. Consultation with a specialist is essential to determine the most appropriate treatment for an individual’s specific case
3. Conventional Surgical Options
The conventional surgical procedure commonly used for treating anal and perianal fistulas is called “fistulotomy.” A fistulotomy is often considered for simple, low-lying fistulas. Here’s an overview of the conventional surgical procedure:
Fistulotomy:
- Procedure: During a fistulotomy, the surgeon makes an incision over the fistula tract, allowing access to the abnormal passageway.
- Cleaning and Excision: The affected tissue and tracts are carefully cleaned and excised, removing any infected or damaged areas.
- Drainage: The wound is left open to allow for drainage, and it is not typically sutured closed. This open wound heals from the inside out.
- Healing: Over time, the wound heals, and the fistula is eradicated. The healing process may take several weeks, and it’s essential to keep the area clean and properly cared for during this time.
- Advantages: Fistulotomy is effective for simple fistulas and often provides a permanent cure. It is a well-established and widely used surgical technique.
It’s important to note that not all fistulas are suitable for fistulotomy. Complex or high-up fistulas may require different surgical approaches, such as seton placement, advancement flap procedures, or more specialized techniques.
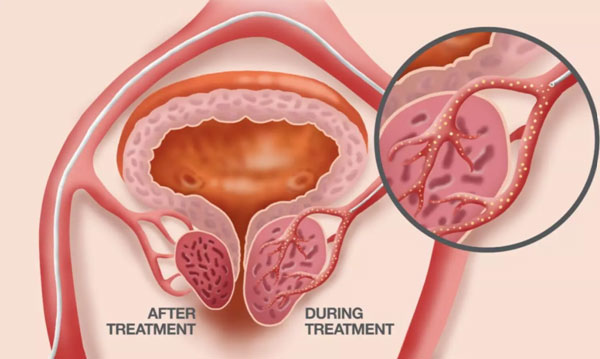
4. Laser treatment for Fistulas
Laser treatment has emerged as a minimally invasive alternative to traditional surgical methods for treating anal fistulas, particularly anal fistulas. This technique has been appreciated for its lower post-operative pain, faster recovery, and lesser risk to the sphincter muscles compared to conventional surgery. Here’s a brief on how the procedure is performed and its benefits:
Procedure:
- A radial emitting laser fiber is introduced into the fistula tract.
- Laser energy is then delivered to the tissue, leading to the obliteration of the fistula tract.
- Over time, the tract shrinks and heals, effectively closing the fistula.
Benefits:
- Minimally Invasive: This procedure is less invasive compared to traditional surgery, which often leads to quicker recovery.
- Sphincter Preservation: Laser treatment has a lesser risk of damaging the anal sphincter muscles, thereby reducing the risk of incontinence, a significant concern in fistula surgery.
- Lower Post-operative Pain: Patients generally experience less post-operative pain and discomfort.
- Faster Recovery: Individuals tend to return to their normal activities quicker compared to traditional surgery.
- Reduced Recurrence Rates: Some studies suggest that laser treatment may have lower recurrence rates, although more long-term data is needed.
Considerations:
- Effectiveness: The effectiveness may vary depending on the type, size, and location of the fistula.
- Cost: Laser treatment can be costlier compared to other forms of treatment.
- Availability: The availability of this treatment might be limited to certain healthcare facilities or regions.
- Long-term Outcomes: More research is needed to fully understand the long-term outcomes and potential complications.
It’s important to consult with a healthcare provider who is experienced in treating fistulas to determine whether laser treatment is a suitable option for your case.
Recovery and Aftercare
Taking certain measures during the days after the surgery will help you have a smooth recovery. Here are a few mentioned below:
- Follow-Up Appointments: Attend all follow-up appointments to allow your healthcare provider to monitor your healing progress and address any concerns.
- Medication Compliance: Take all prescribed medications, including antibiotics and pain relievers, as directed to prevent infection and manage discomfort.
- Wound Care: Keep the surgical area clean and dry, and follow your healthcare provider’s instructions for wound care to promote healing.
- Dietary Modifications: Adopt a high-fiber diet to promote regular bowel movements and prevent straining, which could hinder the healing process.
- Hydration: Drink plenty of fluids to help maintain regular bowel movements and overall health.
- Activity Restrictions: Avoid heavy lifting and strenuous activities as advised by your healthcare provider to prevent any undue pressure on the healing area.
- Sitz Baths: Engage in sitz baths if recommended, to soothe the area and promote healing.
- Physical Therapy: If recommended, participate in physical therapy exercises to strengthen pelvic floor muscles and improve sphincter control
Conclusion
Fistulas represent a challenging medical anomaly necessitating careful treatment and management. The array of treatment approaches ranges from non-invasive measures to surgical interventions, each with distinct advantages and limitations. The advent of minimally invasive techniques like laser treatment showcases the progressive strides in enhancing patient comfort and recovery, albeit with considerations regarding anal fistula surgery cost and long-term effectiveness.
FAQs
1. Which would be the best treatment for fistula?
The best treatment for fistula in bangalore varies per the individual, considering the fistula type, location, and underlying condition. Consulting a healthcare provider for a personalized treatment plan is crucial.
2. Can fistulas heal on their own without treatment?
Rarely, some fistulas may close on their own, but medical or surgical intervention is typically required to treat the underlying cause and prevent complications.
3. How is the success of fistula treatment measured?
Success is measured by the closure of the fistula tract, absence of symptoms, and no recurrence of the fistula or associated infections.
4. How can one prevent infections post-fistula surgery?
Following post-operative care instructions, taking prescribed antibiotics, and maintaining cleanliness around the surgical area can help prevent infections.
5. What are the potential complications if a fistula is left untreated?
Untreated fistulas may lead to recurrent infections, abscess formation, sepsis, and potentially, in rare severe cases, it may lead to cancer.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS