Proctology
Seeking Professional Help: When to Consult a Healthcare Provider for Anal Fistula Treatment

by admin
14th December 2023
7 minutes read
Introduction
Dealing with an anal fistula can be a distressing and painful experience. While the stigma around discussing such conditions may make it challenging to seek help, understanding when to consult a healthcare provider for anal fistula treatment is essential for your health and well-being.
In this blog, we aim to shed light on the critical indicators and signs that should prompt you to seek professional medical care for anal fistulas. By recognizing these red flags and understanding the importance of early intervention, you can take the necessary steps toward effective treatment and recovery. Let’s explore the key reasons why consulting a healthcare provider is vital in managing anal fistulas and regaining your comfort and confidence.
Understanding Anal Fistulas
An anal fistula, a small tunnel-like passage connecting the inside of the anus or rectum to the skin around the anus, is a medical condition that often remains shrouded in silence due to its sensitive nature. To promote a better understanding, it’s essential to unravel the mysteries surrounding anal fistulas.
- Types: There are different types of anal fistulas, such as intersphincteric, transsphincteric, suprasphincteric, and extrasphincteric, each varying in complexity.
- Causes: Anal fistulas typically result from an infection that originates in an anal gland. When the infection fails to drain naturally, it forms an abscess. As the abscess bursts or is drained, a tunnel, known as a fistula, may remain.
- Symptoms: Anal fistulas can cause discomfort, pain, and a range of symptoms, including discharge of pus or blood, itching, and swelling. The intensity of these symptoms may vary.
- Diagnosis: To diagnose an anal fistula, a healthcare provider will typically perform a physical examination and may order additional tests, such as an MRI or a fistulogram.
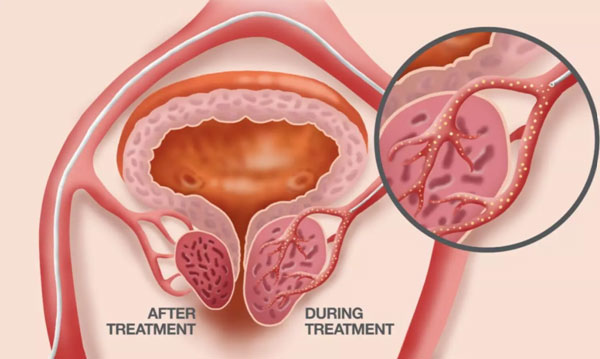
- Treatment: Anal fistula treatment typically involves surgical procedures to remove the abnormal tract and promote healing, with laser treatment for anal fistula as a minimally invasive option for some cases.
Non-Surgical treatment methods such as medications (fistula cure by medicine) and ointments can also provide relief The choice of treatment for anal fistula cure depends on the specific characteristics and complexity of the fistula.
Understanding anal fistulas is the first step toward effective management and treatment. Seeking medical advice is crucial for a timely and accurate diagnosis, ensuring appropriate care for this sensitive condition.
When to Consult a Healthcare Provider for Anal Fistula Treatment
Consulting a healthcare provider for anal fistula treatment is essential when you experience the following signs and symptoms:
Persistent Pain: If you have ongoing or increasing pain in the anal region, it’s time to seek medical attention.
Swelling and Discharge: The presence of swelling, redness, and discharge (often pus or blood) around the anus is a clear indication that a medical evaluation is necessary.
Recurrent Abscesses: If you have a history of abscesses around the anus that keep recurring, it may be a sign of an underlying fistula.
Painful Bowel Movements: If bowel movements are consistently painful or uncomfortable, it’s time to consult a healthcare provider.
Changes in Bowel Habits: Any sudden changes in bowel habits, including constipation or diarrhea, should be discussed with a healthcare professional.
Fever or Chills: The presence of fever or chills, which may indicate an infection, requires immediate medical attention.
Failure to Heal: If an anal fissure or suspected fistula doesn’t heal on its own within a few weeks, it’s crucial to consult with a healthcare provider.
Prior Anal Conditions: If you have a history of anal conditions, such as Crohn’s disease or ulcerative colitis, or if you’ve had an anal fistula before, regular follow-up care is essential.
Family History: A family history of anal fistulas or related conditions may increase your risk, and regular check-ups with a healthcare provider are advisable.
Any Unusual Symptoms: If you notice any unusual or concerning symptoms in the anal region, don’t hesitate to seek medical attention.
Remember that early intervention is crucial in managing anal fistulas effectively. Consulting a healthcare provider allows for a proper diagnosis and the development of an appropriate treatment plan, which may involve surgical procedures or other treatments tailored to your specific condition. Don’t let embarrassment or myths prevent you from seeking the care you need for your health and well-being.
What to Expect During a Medical Evaluation or Anal Fistulas
During a medical evaluation for anal fistulas, you can expect the following steps and procedures:
Medical History: Your healthcare provider will begin by taking a detailed medical history. They will ask about your symptoms, how long you’ve been experiencing them, any previous anal conditions, and any relevant medical conditions or surgeries.
Physical Examination: A physical examination will be conducted, with a focus on the anal and perianal region. Your healthcare provider will check for signs of swelling, redness, discharge, or other symptoms related to the anal fistula.
Digital Rectal Examination (DRE): In some cases, a DRE may be performed. This involves the insertion of a lubricated, gloved finger into the rectum to assess the condition internally.
Imaging Studies: To determine the exact location and characteristics of the anal fistula, imaging studies like an MRI (magnetic resonance imaging) or endoanal ultrasound may be ordered. These tests provide a clearer view of the fistula tract.
Assessment of Underlying Conditions: If an underlying medical condition, such as Crohn’s disease, is suspected, additional tests or blood work may be conducted to assess these conditions.
Consultation: Based on the findings from the evaluation, your healthcare provider will discuss the diagnosis and treatment options with you. They will explain the type of fistula, its complexity, and whether surgical intervention is necessary.
Treatment Plan: If surgical treatment is required, your healthcare provider will discuss the recommended procedure and its potential risks and benefits. They will also provide information about any non-surgical treatment options if applicable.
Preoperative Preparation: If surgery is scheduled, your healthcare provider will provide instructions on how to prepare for the procedure, including fasting, medication management, and other necessary preoperative steps.
Follow-Up: Depending on the type and complexity of the fistula, you may need to schedule a follow-up appointment to monitor your condition and assess the healing process after treatment.
It’s important to communicate openly with your healthcare provider during the evaluation, share any concerns or questions you may have, and actively participate in developing your treatment plan. Seeking timely medical evaluation is essential for an accurate diagnosis and the development of an appropriate treatment strategy for anal fistulas.
Conclusion
Understanding when to consult a healthcare provider for anal fistula treatment and being proactive in seeking medical care can lead to better outcomes and improved anal health. Don’t let myths or stigma deter you from getting the help you need. Remember that early intervention is key, and open communication with your healthcare provider is essential for your well-being. If you suspect you have an anal fistula or are experiencing related symptoms, take the first step and consult doctor for anal fistula in Bangalore.
FAQs
1. Are anal fistulas contagious?
No, anal fistulas are not contagious. They are typically caused by infections but don’t spread from person to person.
2. Is surgery always necessary for anal fistula treatment?
The need for surgery depends on the type, location, and complexity of the anal fistula. While some cases may be managed with non-surgical measures, surgery is often required for a permanent cure, especially for complex fistulas.
3. What is the recovery time after anal fistula surgery?
Recovery time varies depending on the type of surgical procedure performed and individual factors. It can range from a few weeks to a few months.
4. Can anal fistulas come back after treatment?
Yes, anal fistulas can recur, especially if the initial treatment does not fully address the condition. Regular follow-up care is important to monitor healing and prevent recurrence.
5. Are there lifestyle changes that can help prevent anal fistulas?
Maintaining good anal hygiene, avoiding excessive trauma to the anal area, staying hydrated, and including fiber in your diet to prevent constipation can help reduce the risk of anal fistulas.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS