Proctology
How To Know If Laser Surgery For Anal Fissure Is Needed?

by admin
19th December 2023
8 minutes read
Introduction
Anal fissures can be an uncomfortable and sometimes painful condition that many people experience but may hesitate to discuss openly. Treatment provides relief for most cases. Some severe and persistent anal fissures require more advanced treatment. Laser surgery has emerged as one such option for persistent anal fissures. Know if it’s the right choice for you? Learn about the symptoms, benefits, and factors to consider when opting for anal fissure laser surgery from this blog.
Understanding Anal Fissures
The painful cracks or tears inside of the anus lining are called anal fissures. These fissures typically occur when the anal tissues are stretched beyond their normal capacity, often due to constipation, the passage of hard or large stools, or other factors that put excessive strain on the anus. Other potential causes can include anal trauma, inflammatory bowel disease, or sexually transmitted infections. It can result in pain, bleeding during bowel movements, itching, burning, and muscle spasms in the anal region.
It’s essential to consult a healthcare provider if you suspect you have an anal fissure or experience persistent symptoms, as they can provide a proper diagnosis and recommend the most appropriate treatment plan for your specific condition.
Treatment Options For Anal Fissures
The good news is that there are a number of treatment options for anal fissures, ranging from conservative methods to surgical procedures.
1. Home Remedies:
- Warm Sitz Baths: Soak in a warm tub or a sitz bath several times a day for 10-20 minutes each. The warm water helps to relax the anal muscles and the added salt helps to promote healing.
- Fiber Intake: Fiber helps to soften the stool so that the bowels do not have to work as hard and will not cause a lot of pressure on the hemorrhoids.
2. Topical Medication:
- Nitroglycerin: Nitroglycerin ointment helps with healing by increasing blood flow to the fissure and reducing pain.
- Topical Anesthetics: These creams reduce the feeling of pain. Lidocaine is the most common anesthetic used and it provides temporary relief.
- Calcium Channel Blockers: These medications relax the anal sphincter muscles and relieve anal pressure.
3. Botulinum toxin: Botulinum toxin (Botox) injections can paralyze the anal sphincter muscle, lowering discomfort and accelerating recovery.
4. Surgical Options:
- Lateral Internal Sphincterotomy (LIS): This outpatient procedure is the most common surgery for patients with chronic fissures. A small incision is made to partially cut the anal sphincter muscle which reduces its tension and promotes healing.
- Fissurectomy: The doctor removes the fissure tearing muscle sphincter and exposes the underlying muscle tear which is allowed to heal as a fresh wound and thus promotes healing.
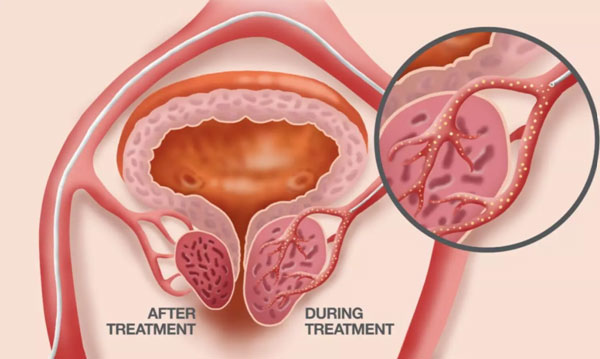
- Fissure laser surgery: A fissure surgical option, using a laser. The benefits of the procedure include reduced postoperative pain and faster healing than traditional meds, with a reduced risk of incontinence.
Before deciding on a course of treatment, always seek the advice of a healthcare expert. They may offer advice that is specifically catered to each person’s requirements and situation. Here, let’s understand laser surgery for anal fissures in detail.
How Does Laser Surgery Work For Anal Fissures?
Laser surgery for anal fissures offers a newer, minimally-invasive treatment for this painful condition. Traditional methods may involve more invasive surgical techniques or take longer for recovery when compared with laser technique.
During laser surgery for anal fissures, a surgeon uses a specialized laser, often a carbon dioxide (CO2) laser, to precisely cut and seal the fissure. This is usually done on an outpatient basis, and the patient may be under local anesthesia or general anesthesia, depending on the case and surgeon’s preference.
The laser is used to make a controlled incision in the internal anal sphincter muscle, which is the muscle that surrounds the anal canal. This incision helps relax the muscle and reduce spasms, which are a common cause of pain and discomfort in anal fissures. Simultaneously, the laser’s energy seals the blood vessels and nerve endings, minimizing bleeding and post-operative pain.
The perks of laser surgery include comparably less pain after the surgery, recovery at a faster pace, and risks that are virtually minimal. The laser is so precise in vaporizing target tissue and affecting haemostasis that it causes little damage and therefore elicits little pain to surrounding tissues.
When is Laser Surgery For Anal Fissures Recommended?
Laser treatment for anal fissures is a high-tech, minimally invasive treatment. Here are the indications for laser treatment:
- Chronic Fissures: Most anal fissures heal with at-home treatment (sitz baths, increased dietary fiber, ointments) in a few days or a few weeks at most. A small number of fissures fail to heal (persisting for weeks) or continue to recur and are considered “chronic.” These might benefit from a surgical procedure that permanently shuts off or resurfaces the neural pathways in the anus that regularly transmit pain signals to the brain.
- Failed Conservative Treatments: Surgery is a last resort after non-surgical treatment measures, including prescription-strength topical nitroglycerin, oral calcium channel blockers, or Botox injections, fail to provide relief or if the fissure heals and then comes back.
- Severe Pain or Discomfort: Surgical intervention can be all the more appealing when the pain or discomfort is so intense that it becomes debilitating and affects your daily activities.
- Complications to Associate: Anal fissures may be associated with other complications such as a skin tag (sometimes called sentinel pile) or an abscess. In such situations, the surgeon can address both the fissure and the related complication by putting the patient under laser surgery.
- Patient’s preference: Some patients want to go for an invasive procedure (Laser Surgery) as it offers some advantages such as reduced post-operative pain and early recovery. They want to get back to their normal lifestyle and are worried about the pain that traditional open anal fissure surgery carries.
- Expert Recommendation: The choice of treatment can vary depending upon the choice of your surgeon. Based on the examination of the fissure, the depth of the fissure, its location, and other factors the doctor may recommend for open fissure surgery (laser surgery).
It is important to note that the decision for fissure surgery by laser should be made in collaboration with a healthcare professional who can evaluate the unique situation and recommend the most appropriate treatment option.
When to Avoid Laser Fissure Surgery?
While laser surgery is an efficient method used to repair fissures, there are instances when it may not be conducted. Here are situations in which laser surgery for anal fissures may be avoided.
- Acute fissures: If an anal fissure is new, meaning it’s been there for less than six weeks, it is called an “acute” fissure. These acute fissures tend to heal well with conservative treatment and rarely require any surgical intervention.
- Underlying medical conditions: Patients with medical conditions such as Crohn’s or other inflammatory bowel diseases are not good candidates for any surgery, including using the laser. The underlying problem needs to be addressed before considering laser surgery.
- Infection: If there is an active infection in or near the anus, it would make sense to treat that problem before considering laser surgery.
- Anatomic problems: Some patients may have abnormalities, such as anal fistulas or other conditions that make the use of a laser less attractive.
- Limited Availability: Not all medical facilities have the necessary equipment and trained surgeons for this procedure. It is important to ensure that the provider chosen has experience with laser surgery for anal fissure.
- Cost: The cost of laser surgery may be higher than other surgical treatments when considering healthcare coverage and location. It is important to consider the cost and understand your insurance coverage before making a decision.
- Previous Surgeries: Patients that have had multiple surgeries in the anal area may have scar tissue or anatomy that is different and may make the surgery with the laser difficult.
A comprehensive discussion with a healthcare provider is important so that patients can evaluate the potential benefits and risks of each treatment approach and determine which one is right for them.
Conclusion
Laser surgery provides a new option for patients with an anal fissure who do not want to have a traditional fissure operation or fissure surgery. Not everyone is an appropriate candidate for surgery; health, the nature of the anal fissure, and personal factors should be considered. Always check with your anal fissure specialist in Bangalore for the best approach to your condition and the best way to ensure fast healing and comfort.
FAQs
1. Is an anal fissure the same as hemorrhoids?
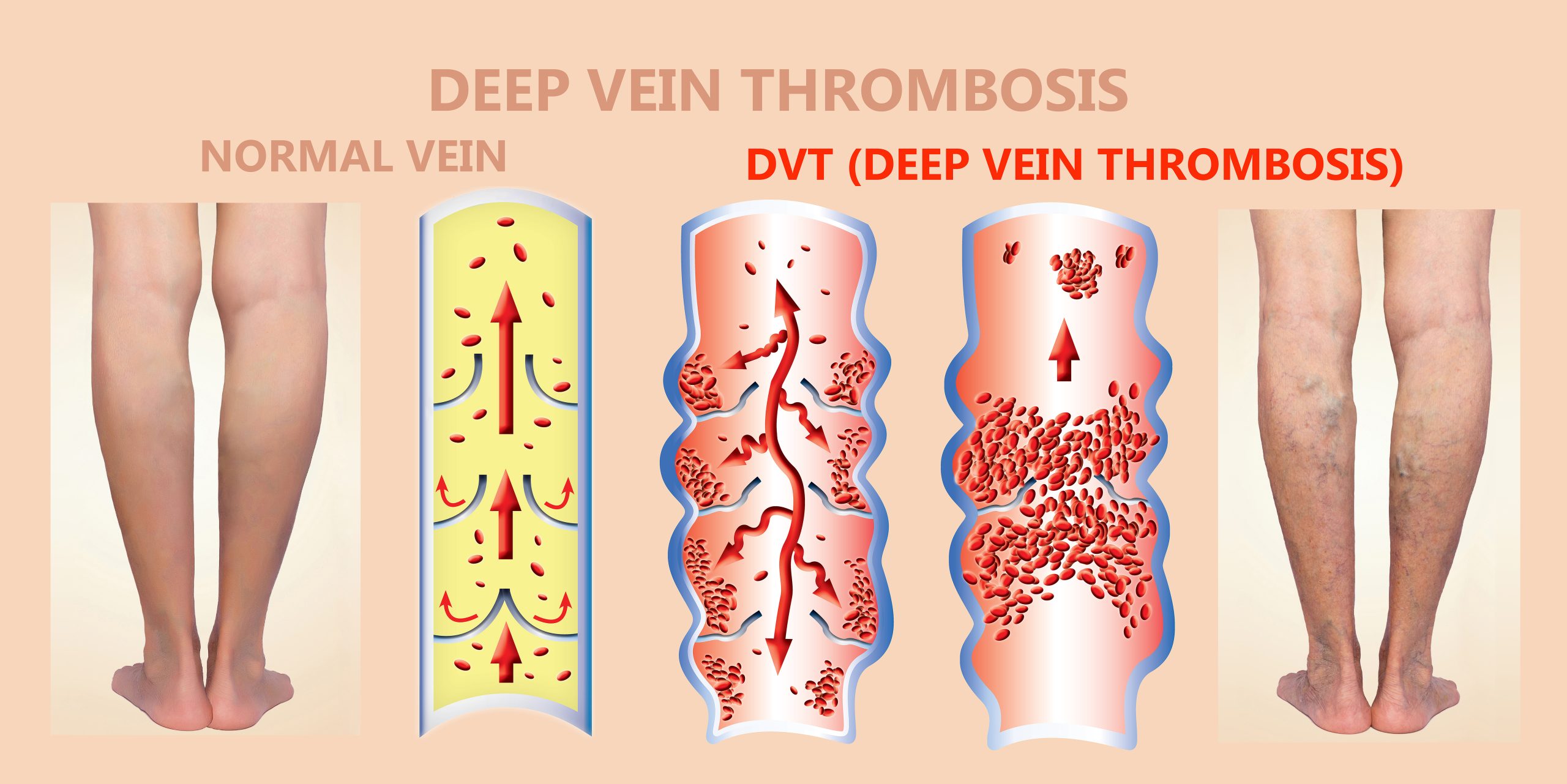
No. While both can cause anal pain and bleeding, they are distinct conditions. Hemorrhoids are swollen blood vessels in the rectum or anus, while fissures are tears in the anal lining.
2. Do anal fissures bleed?
Yes, one common symptom of an anal fissure is bright red blood on the toilet paper or in the stool after a bowel movement.
3. Can I use over-the-counter creams for relief?
Over-the-counter creams can provide temporary relief from pain or itching. However, it’s essential to consult a physician for persistent symptoms.
4. Will I need multiple laser treatments for my fissure?
Typically, one laser treatment session is sufficient for treating an anal fissure. However, the requirement varies depending on the individual’s healing and the fissure’s severity.
5. Can anal fissures lead to cancer?
No, anal fissures are benign and don’t increase the risk of cancer. However, persistent symptoms should be evaluated by a physician to rule out other conditions.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Health
- Health Insurance
- Hernia
- Hindi
- Hip Arthoscopy
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Urology
- Uterine Artery Embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS