Paraphimosis / Uncategorised
Paraphimosis: Symptoms, Causes, Diagnosis, and Treatment
by admin
4th October 2023
7 minutes read
Introduction
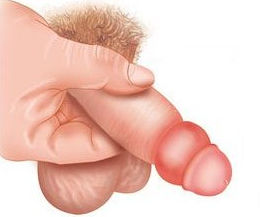
Paraphimosis is a urological emergency where the foreskin of an uncircumcised male is retracted behind the glans penis and cannot return to its original position. This constriction impedes blood flow, potentially leading to glans tissue damage. Causes may include forceful foreskin retraction or sexual activity. Symptoms encompass swelling, pain, and a tight band of foreskin behind the glans. Prompt diagnosis is crucial to prevent complications. Treatment usually involves manual reduction to reposition the foreskin or surgical intervention in severe cases. It’s essential to distinguish paraphimosis from phimosis, where the foreskin cannot be retracted at all.
What is Paraphimosis?
Paraphimosis is a medical condition in uncircumcised or partially circumcised males where the foreskin, once retracted behind the glans penis, cannot be returned to its original position. This situation can lead to the constriction of blood flow to the glans penis. If left untreated, it can result in swelling, pain, and even tissue damage or gangrene of the glans due to reduced blood circulation.
What are the Causes and Risk Factors?
Paraphimosis is primarily caused by the retraction of the foreskin behind the glans penis without it being returned to its natural position. Several scenarios or conditions can lead to or increase the risk of paraphimosis:
- Medical Examinations and Procedures: If the foreskin is retracted and not replaced during medical examinations, catheter insertions, or other procedures.
- Forceful Retraction: Overzealous or forceful pulling back of the foreskin can lead to paraphimosis, especially in boys whose foreskin hasn’t fully separated.
- Sexual Activity: The foreskin can become trapped behind the glans after sexual activity, especially if not returned to its natural position post-activity.
- Swelling or Infections: Conditions like balanitis (inflammation of the glans) or other infections can cause swelling that makes it difficult for the foreskin to return over the glans.
- Prolonged Retraction: For instance, if someone retracts the foreskin for cleaning and forgets to replace it.
What are the Symptoms of Paraphimosis?
Paraphimosis is characterized by a set of distinctive symptoms, and recognizing them promptly can expedite medical intervention and reduce the risk of complications. The primary symptoms of paraphimosis include:
- Swelling: The glans penis (head of the penis) and the foreskin may become noticeably swollen.
- Pain: The affected individual may experience significant pain or discomfort in the penis, particularly in the glans area.
- Tight Band: A constricting band of foreskin can be seen or felt behind the glans, which is essentially the retracted and trapped foreskin.
- Discoloration: The glans might appear darker in color due to the reduced blood flow. In severe cases, it may turn blue or black, indicating a critical lack of circulation that can lead to tissue death.
- Difficulty Urinating: Some men might experience difficulty or pain while trying to urinate.
How is Paraphimosis Diagnosed?
The diagnosis of paraphimosis is primarily clinical, based on physical examination and the patient’s medical history. Here’s how the condition is typically diagnosed:
- Physical Examination: The most definitive way to diagnose paraphimosis is by visually inspecting and physically examining the penis. A healthcare provider will look for the telltale signs: the constricting band of foreskin trapped behind the glans, swelling of the glans and foreskin, discoloration, and other aforementioned symptoms.
- Medical History: The doctor will ask about recent activities or events that might have triggered the condition, such as medical procedures, forceful retraction of the foreskin, or sexual activity.
- Differentiation from Phimosis: It’s essential to differentiate paraphimosis from phimosis. While both conditions involve the foreskin, phimosis is when the foreskin cannot be retracted over the glans, while paraphimosis is when the retracted foreskin cannot be returned to its original position.
What is the Treatment for Paraphimosis?
The treatment for paraphimosis aims to reduce the swelling and return the foreskin to its natural position covering the glans. Here are the common approaches for treating paraphimosis:
1. Manual Reduction:
This is the first-line treatment.
- Osmotic Method: Applying a hypertonic solution (like mannitol) or granulated sugar to the swollen area can help draw out fluid and reduce swelling.
- Compression: Gentle but firm pressure is applied to the glans to push out the accumulated blood and edema, followed by moving the foreskin over the glans.
2. Pain and Swelling Management:
Painkillers and cold compresses can be used to manage pain and reduce swelling, making manual reduction easier.
3. Puncturing Technique:
In cases where the swelling is severe, a doctor might make multiple small punctures in the foreskin to release fluid and alleviate edema, facilitating manual reduction.
4. Surgical Intervention:
In rare cases where manual reduction fails or if there’s tissue necrosis (dead tissue due to lack of blood supply):
- Dorsal Slit: A surgical incision is made along the top of the foreskin to relieve the constriction.
- Circumcision: If recurrent episodes of paraphimosis or other complicating factors are present, circumcision, which is the complete removal of the foreskin, might be recommended.
Preventive Methods
Preventing paraphimosis largely involves understanding its causes and ensuring appropriate care and handling of the foreskin. Here are some preventive methods:
1. Proper Foreskin Care:
- Always return the foreskin to its natural position covering the glans after retraction.
- Avoid forceful retraction of the foreskin, especially in young boys whose foreskin might still be naturally adhered to the glans.
2. Educate about Risks:
Medical professionals, caregivers, and individuals should be educated about the risks associated with leaving the foreskin retracted for extended periods. This is particularly crucial during medical examinations or procedures.
3. Routine Genital Hygiene:
Regular, gentle cleaning under the foreskin can prevent infections like balanitis which can predispose to paraphimosis.
4. Consider Circumcision:
While a personal and often culturally influenced decision, circumcision eliminates the risk of paraphimosis. It’s important to understand the risks and benefits.
5. Promptly Address Infections or Swelling:
Conditions like balanitis or edema should be treated promptly to reduce the risk of developing paraphimosis.
6. Awareness During Intimacy:
Being aware during sexual activity, ensuring that the foreskin doesn’t remain trapped behind the glans afterward.
7. Cautious with Piercings:
If considering genital piercings, be informed about potential risks and ensure they are done by professionals familiar with the anatomy and potential complications.
8. Use Lubrication:
If the foreskin tends to be tight or gets stuck occasionally, using lubrication during retraction can help in smoother movement.
Conclusion
Paraphimosis is a urological emergency that arises when a retracted foreskin cannot return to its original position, potentially impeding blood flow to the glans penis. Awareness and proper foreskin care are paramount in prevention. Early recognition of symptoms and immediate medical intervention are crucial to prevent complications. By understanding its causes, practicing preventive measures, and prioritizing genital health, the risks associated with paraphimosis can be significantly mitigated.
FAQs
While paraphimosis can occur at any age, it’s less common in older men compared to children and younger adults, mainly due to the natural separation of the foreskin from the glans with age.
Yes. Delay in treatment can lead to reduced blood flow, tissue damage, and in severe cases, necrosis (tissue death) of the glans.
No. Home remedies or OTC products are not recommended. Immediate medical intervention is necessary.
No. Many cases can be managed with manual reduction. Surgery is reserved for severe cases or when other methods fail.
Post-procedural swelling is generally even and doesn’t involve a constricting band of foreskin behind the glans. If in doubt, always consult a healthcare professional.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
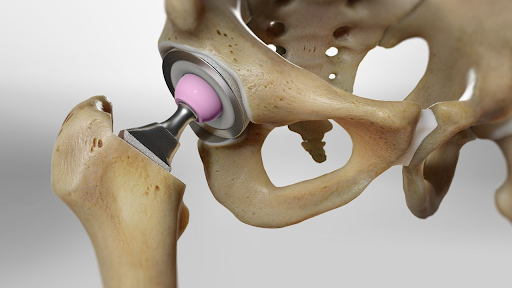
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
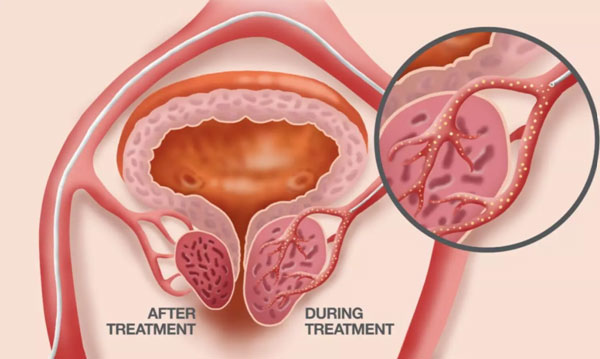
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS