Government Schemes
Mahatma Jyotiba Phule Jan Arogya Yojana

by admin
23rd November 2023
4 minutes read
All over the country, state governments are coming up with schemes/policies to help poor families get healthcare services free of cost. Mahatma Jyotiba Phule Jan Arogya Yojana (MJPJAY) is also one of such schemes launched by the Maharashtra government. This health insurance cover was originally Rajiv Gandhi Jeevandayee Arogya Yojana, which was renamed in April 2017.
The scheme aims to provide quality medical insurance access at affordable prices. It is for those below the poverty line (yellow ration card) and marginally above the poverty line (orange ration card) policyholders. It also provides a surgicare cover against various surgical procedures.
Features of the Mahatma Jyotiba Phule Jan Arogya Yojana
- The premium charges required to avail of this scheme are paid by the state government
- Policyholders can receive health insurance benefits for up to a sum insured limit of Rs. 1.5 lakhs/year
- The insurance benefit can be enjoyed by an individual or an entire family on a floater basis
- There’s no waiting period for pre-existing diseases
- Health insurance benefits are received in the cashless form and no deposit is required to get treated under the policy
- The policy covers surgeries, diagnosis, follow-up treatment and medications
- The official website consists of the names of network hospitals, both government and private
- To enrol for this scheme, one may visit a nearby network hospital and file an application
- The scheme further allows access to one free medical camp/year to the beneficiaries (conducted in taluka headquarters, municipalities and major gram panchayats)
Benefits of the Mahatma Jyotiba Phule Jan Arogya Yojana
- The scheme covers around 971 types of surgeries/therapies/procedures in 30 identified specialized categories
- The scheme covers around 121 types of follow-up procedures in 30 identified specialized categories
- Diagnosis, follow-up consultation, medicines, etc. are covered for up to 10 days post-discharge from the hospital
- Some of the categories covered for surgeries – plastic surgery, cardiology, ENT surgery, neurology, burns, radiation therapy, infectious diseases, critical care, etc.
- Around 132 types of government-reserved procedures (to be performed only in empanelled government hospitals/medical colleges)
- Renal failure is covered with an upper limit of Rs. 2.5 lakhs/operation
Talking of what is not covered by the scheme, there are no such outright exclusions provided. For instance, conditions like appendicitis and hernia will not be covered unless it’s an emergency.
MJPJAY Beneficiaries
The following is a list of MJPJAY beneficiaries:
- Families holding Yellow ration card, AAY or Antyodaya Anna Yojana ration card, Orange ration card (annual income up to Rs. 1 lakh) for 36 districts of Maharashtra
- White ration cardholder farmer families from 14 agricultural distressed Maharashtra districts
- Students of Government Ashram Shala, children of government orphanages, senior citizens of government old age homes and female inmates of Government Mahila Ashram
- Journalists and their dependent family members (approved by DGIPR)
- Construction workers as well as their families, who have live registration with the Maharashtra Building
Claim Procedure for Mahatma Jyotiba Phule Jan Arogya Yojana
To receive treatment, one needs to visit an empanelled hospital and talk to any of the Arogyamitras placed in the hospital. S/he will examine your valid ration cards and photo ID.
The claim procedure begins with the diagnosis of the condition. If the diagnosis is made in a network/empanelled hospital, treatment will immediately begin after getting pre-authorization. However, if the hospital is not a network hospital, a referral card is given to start treatment in a nearby network hospital. Furthermore, network hospitals can now get E-preauthorization from the insurer after filing an online request.
Treatment begins after pre-authorization is obtained from the insurer. Once, the cashless treatment and surgery are completed, the network hospital sends all relevant documents (including medical bills, diagnostic reports, and discharge summary) to the insurer. The insurer then verifies all documents and gives approval for the claim settlement to the network facility.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
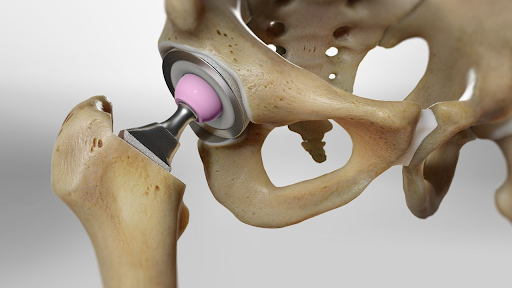
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
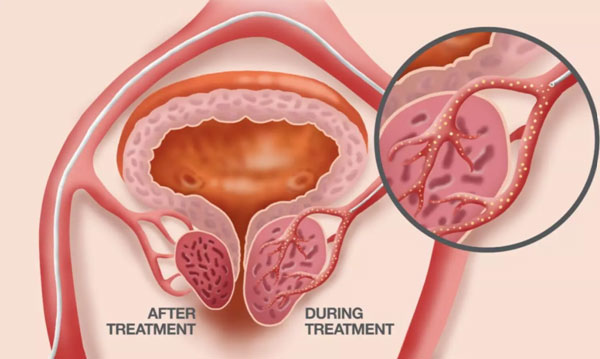
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS