Government Schemes
Dr YSR Aarogyasri Health Care Trust Andhra Pradesh State Government
by admin
23rd November 2023
7 minutes read
The Dr. Aarogyasri Health Care Trust, presided over by the chief minister, was established by the state government of Andhra Pradesh to aid the implementation of the Dr. YSR Aarogyasri Health Insurance Scheme. The trust operations are overseen by a chief executive officer with an IAS officer designation.
So, what is the Dr. YSR Aarogyasri Health Insurance Scheme?
It is a state-sponsored scheme (launched in 2007 by the government of Andhra Pradesh) whose aim is to achieve universal health coverage for the BPL (below poverty line) families in terms of financial security and access to healthcare. It also aims to offer trustworthy, high-quality and evidence-based healthcare services. It’s a PPP model (public-private partnership model) for health insurance, meant for low-income families.
Moreover, the scheme offers complete cashless services for diseases that fall under secondary and tertiary care. It further involves free screening and outpatient consultation in health camps and network hospitals.
Coverage Under the Dr. YSR Aarogyasri Scheme
The scheme covers various treatments, namely – cardiac and cardiothoracic surgery, cardiology, nephrology, neurology, neurosurgery, ophthalmology surgery, organ transplantation surgery, cochlear implant surgery, critical care, dermatology, endocrinology, ENT surgery, epidemic disease, gastroenterology, general medicine, general surgery, orthopaedic surgery and procedures, paediatric surgeries, paediatrics, plastic surgery, poly trauma, psychiatry, pulmonology, radiation oncology, infectious disease, medical oncology, genito urinary surgeries, gynaecology and obstetrics surgery, surgical oncology, surgical gastroenterology and rheumatology.
Procedures not covered under the scheme include the following – gamma-knife procedures in neurosurgery, assisted devices for cardiac failures, tuberculosis, medical treatment for bone marrow, filaria, HIV/AIDS, infectious diseases, jaundice, cardiac and liver transplantations, surgery for knee replacement, gastroenteritis, malaria and leprosy.
Features and Benefits of the YSR Aarogyasri Health Insurance Scheme
- In-patient care is provided for all diseases covered under the scheme
- Out-patient treatment can be taken at health camps and in the network hospitals
- The allocated sum insured is applicable to the entire family and no member has to buy the plan separately
- The scheme covers pre-existing illnesses that a beneficiary already had before enrolling in the programme
- Financial protection given is worth Rs. 5 lakhs/family/year
- The scheme also covers follow-up procedures after hospitalization
The objectives of the scheme include providing free quality hospital care to BPL families, strengthening government hospitals through demand-side financing and giving universal health coverage to both urban and rural poor of the state.
The following services are provided free of cost – admission to the hospital, doctor consultation (every day), nursing services/day, necessary medical tests and medicines, surgery/treatment, breakfast and lunch (2 meals), medicines for 10 days post-discharge and necessary transportation charges to go back home post-discharge.
Who Is Eligible For Dr. YSR Aarogyasri The Scheme?
- Individuals with a rice card
- Families qualified for the YSR Pension Kanuka Card as well as Jagananna Vidya and Vasathi Deevena Card
The following criteria apply to the other families:
- Landowners with less than 12 acres of wetland
- Landowners with less than 35 acres of dry land
- Landowners with 35 acres of land in total
- Municipal Property Tax Payers – households paying municipal property taxes for an area of less than 3,000 square feet (334 square yards)
- Households with only one personal car
- An employee (not a permanent government employee/pensioner) with a salary lower than or the same as Rs. 5 lakhs/year. This includes outsourcing, part-time employees, contract workers, sanitary workers and honorarium-based employees of the government sector and private sector employees
- Families with maximum Rs. 5 lakhs as their annual income (as shown in their salary certificates)
- Lastly, families/households that file income tax returns for a maximum annual income of Rs. 5 lakhs (as shown in their income tax return evidence)
Dr. YSR Aarogyasri Scheme: Claim Procedure
The claim process is as follows:
For Beneficiaries: Upon enrolment, the beneficiaries are given YSR Aarogyasri health cards. The patient only has to present this card to the Vaidya Mitra (a facilitator) at the empanelled/network hospital to receive medical care. The treatment starts once the data listed on the card is gathered.
Moreover, if the patient does not have the card, s/he can share their card number with Vadiya Mitra. Information can also be obtained from the Aarogyasri Trust, if documentation is not available to confirm the patient’s eligibility for the scheme.
For Hospitals: The hospital needs to request pre-authorization in case of planned surgical treatments. For the Trust to accept the claims, the hospitals should fulfil the following requirements:
- Claim intimation on time
- Photographic proof of the treatment
- The claim amount up to the pre-authorization limit
- Pre-authorization to perform a listed treatment
A claim is settled with the assistance from the Dr. Aarogyasri portal. The portal further helps in gathering claim documents, notifying claims and reviewing claim documents. After the receipt of the claim, the following verifications are carried out:
- Identity of the patient
- Proof of treatment
- It is verified that the claim amount is in line with the pre-authorization amount
- Management of cases as per the pre-authorization
The Trust confirms the applicant’s identity, the amount of claim, the listed therapy and the supporting documents. Claim settlement and payment to the network hospital need to be done within 7 days of confirmation.
What Documents Are Required For the Dr. YSR Aarogyasri Scheme?
Documents needed include:
- Address proof
- Aadhaar card
- Income tax returns or income certificate
How to Apply for the Dr. YSR Aarogyasri Scheme Online
- First, get registered on the gram ward Sachivalayam portal or YSR Navasakam’s official website
- Select ‘Login’ to get a new page on the screen
- Click the ‘Aarogyasri Health Card’ application form
- Fill out the necessary information and upload all required documents
- Finally, you can submit the application form and get a printout for a record
How to Apply for the Dr. YSR Aarogyasri Scheme (Offline)
- Visit the official website of YSR Navakaram
- Under the ‘Download’ section, select ‘YSR AArogyasri Health Card Performa’
- Download the displayed application form, collect the printout and fill it with your details
- Submit the completely filled form with supporting documents to the concerned department. The authorities will verify the same and issue you a YSR Health Card
The YSR Aarogyasri Health Card
This is a card given to the eligible families who enrol in the scheme. It is through this card, that you receive cashless medical services at the empanelled hospitals. The card has your unique card number and photo. During medical emergencies, the card can serve as a document of enrolment.
How to Download the YSR Aarogyasri Health Card?
- Visit www.ysraarogyasri.ap.gov.in and under the ‘EHS’ section, click ‘Download Health Card’
- Enter your user ID and click ‘Go’
- Fill out the form and your card will appear on the screen; you can download the same for future
A Few Points to Note
- For assistance, one can get in touch with the Aarogya Mitras available at the empanelled hospitals; one can further reach out to a health camp conducted by a network hospital or use the 24-hour call centre service through 104 (toll-free number)
- The premium for the scheme is entirely paid by the Andhra Pradesh government on behalf of the BPL families
- All BPL families with active white ration cards are covered under this scheme from the day of the implementation of the scheme
- Post-enrolment, one can avail of the scheme’s benefits by going to a PHC/CHC/area hospital/district hospital or any nearby government hospital/health camp; you will need to carry your white card/health card and medical reports if any (any network hospital can be reached out during emergency)
Conclusion
Recently, the YSR Aarogyasri Health Care Trust assured the clearing off of all payments due to private hospitals. It continues to accept new patients as well. By now, Rs. 368 crores have already been paid to provide healthcare services at all network hospitals.
CATEGORIES
- ACL Reconstruction
- Anal Fissures
- Anal Fistula
- Appendicitis
- ASK A DOCTOR
- Benign Prostatic Hyperplasia
- Breast Lump Excision
- Cataract
- Circumcision
- Conditions & Diseases
- Cosmetology
- Covid-19
- Cure
- Endocrinology
- ENGLISH VIDEOS
- Eye Care
- Gallstones
- General Surgeries
- Government Schemes
- Gynaecology
- Gynecomastia
- Health
- Health Insurance
- Hernia
- hindi
- Hip Arthoscopy
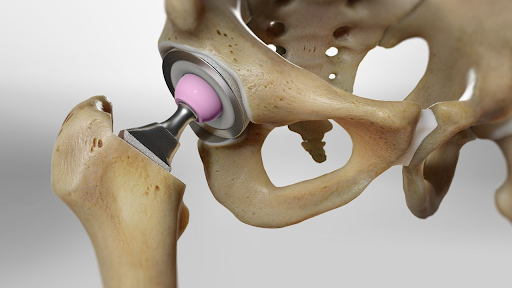
- Hip Replacement
- Hip Replacement Surgery
- Hydrocele
- Kannada
- Kidney Stones
- Knee Arthroscopic
- Laparoscopic
- LASER
- Latest Treatments
- Lifestyle
- Liposuction
- Medfin Stories
- Medicine
- Nephrology
- Ophthalmology
- Orthopaedic
- Paraphimosis
- Patient Testimonials
- PCL Reconstruction
- Phimosis
- Piles (Hemorrhoids)
- Pilonidal Sinus
- Proctology
- Prostate Artery Embolization
- Rhinoplasty
- Second Opinion
- Total Knee Replacement
- Uncategorised
- Urology
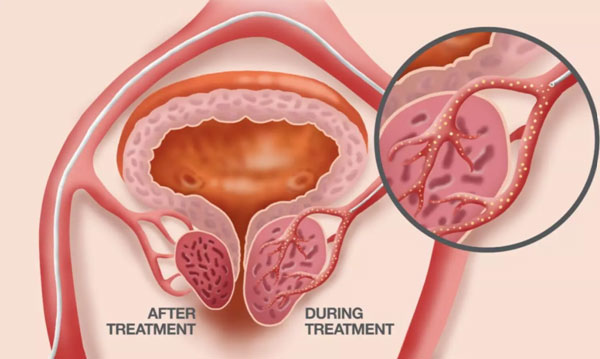
- uterine artery embolization
- Uterine Fibroids
- Varicocele
- Varicose Veins
- Vascular
- VIDEOS